Organoids generated from tonsils removed during surgeries provide a reliable in vitro platform to study human immune responses.
For many people, getting their tonsils removed is a childhood memory: a sore throat, a surgery, some ice cream, and skipping school. More than half a million people undergo tonsillectomies each year in the US to treat recurrent throat infections and sleep-disordered breathing conditions.1 But the olive-sized tissues are more than just troublemakers; they are lymphoid organs where immune cells mature.

“Kids are having tonsillectomies all the time, and [the tonsils] are just loaded with T and B cells,” said Lisa Wagar, now an immunologist at the University of California, Irvine. This prompted Wagar, at the time a postdoctoral researcher at Stanford University working with immunologist Mark Davis, to explore using excised tonsils, which surgeons would otherwise discard, as starting material for generating immune organoids.2
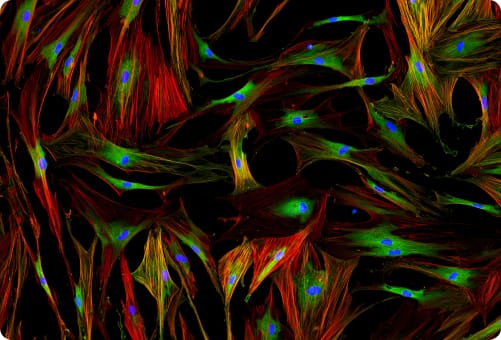
In 2021, Wagar and Davis demonstrated that their system mimicked cellular interactions and organization observed in tonsils, providing an in vitro platform to study immune responses. Since then, researchers, including Wagar and Davis, have used these tonsil organoids to investigate vaccine responses, lymphocyte functions, and infections such as SARS-CoV-2.3-5
Seeing so many researchers using the tonsil organoids for various purposes “has been exciting,” said Wagar. “I’m just super happy to see people using a tool that I developed for my own purposes.”
Tonsil Organoids Offer a Platform to Study Human Adaptive Immune Responses
To develop these tonsil organoids, Wagar, Davis, and their team borrowed an approach that another group used to generate thymic organ cultures.6,7 They broke down tonsils into their constituent cells and allowed these to reaggregate in culture, giving rise to organoids.

Then, they studied the immune responses in the lymphoid organoids. Exposing them to an influenza vaccine caused B cells to mature and eventually secrete influenza-specific antibodies. When the researchers peeked into the structure of antigen-exposed tonsil organoids, they observed organization of lymphocytes in patterns consistent with those found in lymphoid organs undergoing an adaptive immune response.
Additionally, the group saw that the organoids supported key lymphoid organ functions including somatic hypermutation, wherein immunoglobulins accumulate mutations to produce antibodies with enhanced antigen-binding affinity. Wagar and Davis also successfully trialed the organoids against SARS-CoV-2 vaccine candidates, where they saw the cultures secreting specific antibodies.
With these findings, the team showed that the system captured key lymphoid organ features and offered an in vitro preclinical platform to study human immune responses. Their work provided an alternate tool for other scientists who had largely relied on mouse models, which may not always translate well to human tissue, for their studies. Equipped with human lymphoid organs in a dish, researchers set out to answer several questions.
Tonsil Organoids to Study the Immune System and Vaccine Responses
During the COVID-19 pandemic, researchers used tonsil organoids to investigate the genetic and metabolic changes that SARS-CoV-2 triggered. They also evaluated antiviral drugs on the platform.5 Soon after, Wagar and her team used the organoids to understand how different influenza vaccine antigens trigger distinct magnitudes, populations, and functions of lymphocytes, highlighting that the organoids could be used to study vaccine design.3
Scientists have also turned to the organoids beyond vaccine studies. “There’s people using them for the basic biology of tissue-resident immune cells,” said Wagar. Using the organoids, scientists discovered that a class of regulatory T cells originate from two different cell lineages, which could guide new treatments for autoimmune diseases.8 Davis and his team used tonsil organoids to tease out how different subsets of T cells cooperate with each other to help prevent an autoimmune response.4
Despite its usefulness to study human immune responses in vitro, the organoid model is not exhaustive. For instance, the system cannot fully recapitulate the cellular interactions that take place in vivo. “[It is a] good idea for us to try to continue developing our in vitro models,” said Wagar. “But where we are right now, we’re still very far away from modeling the immunology of a whole animal.”
Wagar noted that scientists are working towards building immune organ-on-a-chip systems containing cells and perfused chambers that can more accurately mimic the tissue-level physiology.
But overall, Wagar noted that the tonsil organoids solved a major challenge in studying human immunology, which was limited to observational rather than experimental studies. “Having a platform where [doing mechanistic experiments] is possible really was transformative for me,” said Wagar. “Seeing all these amazing tools that are out there for animal models and being able to ask those mechanistic questions [in humans] and answer them, has been very exciting.”